Building Community Through Storytelling: A Case Report
By Ndidiamaka D. Matthews, PT, DPT; Shreya Jain, PhD; Joshua Limlingan PT, DPT
Introduction
Physical therapy plays a leading role in patient-centered care, where physical therapists have the unique ability to transform patients’ lives by helping them restore mobility, build confidence, and regain independence. However, the profession faces significant diversity challenges in the United States, with 82.6% of physical therapists identifying as White compared to 58.9% of the population (US Bureau of Labor Statistics, 2020 US Census). This lack of diversity can result in potential gaps in empathy, tolerance, and understanding between physical therapists and the patients they serve. It may also impact the sense of belonging among physical therapists from underrepresented groups, who might struggle to find role models or colleagues with similar experiences and perspectives.1,2
Storytelling—the sharing of ideas, beliefs, and struggles of individuals through narratives—offers a powerful way to address some of these challenges by providing a platform for diverse voices to be shared and appreciated.3 Although the potential of storytelling for physical therapists has been recognized, no specific intervention has yet been developed.4
Storytelling has been a fundamental part of the human experience for millennia, yet it has only been recognized as a therapeutic tool by Western medicine in the past 40 years.5,6 More recently, storytelling has been used to improve psychological and physical well-being and to build more cohesive communities that appreciate diverse perspectives.4,7–9
In educational settings, stories can empower students to share experiences in a non-judgmental environment while developing important skills such as communication and attentive listening.9 Specifically in healthcare education, sharing and listening to personal stories can help healthcare professionals be better equipped to care for their patients by attuning them to their patients’ stories and journeys with illness.10–12 Storytelling events and activities prompt reflection among faculty, clinical instructors, and students, allowing the listener to gain insight into others’ experiences—ultimately fostering supportive environments and encouraging compassion and empathy.7–9
Recognizing the numerous benefits of storytelling in healthcare and education, the USC Division of Biokinesiology and Physical Therapy has hosted four annual ‘StorySlam’ events over the past five years. Our purpose in this article is to share details of our most recent StorySlam, with the hope of encouraging similar events in physical therapy education. Additionally, we seek to evaluate how this event has impacted the sense of belonging among Division members and contributed to strengthening our community.
Methods/Event Description
The Diversity, Anti-Racism, Inclusion, and Community Engagement Council of the University of Southern California Division of Biokinesiology and Physical Therapy wanted to create a space where people could come together and share their personal stories. They had been inspired by the Annals of Internal Medicine ‘Story Slam’ series, and thought “We could do that.”13 That’s how the idea of the USC StorySlam was born.
The goal of the StorySlam was simple: to give Division members a platform to share their own experiences—stories that reflected their encounters with equity, diversity, and inclusion. But the StorySlam wasn’t just about talking; it was about listening, building connections, and creating a stronger sense of community. The organizing committee wanted people to walk away feeling like they belonged to something bigger. As Spring 2023 approached, the event began to take shape. Faculty, staff, and student storytellers were excited to share their experiences in front of their peers, both in-person and virtually.
The Build-Up
Three months before the event, the organizing committee sent out a call to all faculty, staff, students, and even alumni who had participated in diversity initiatives. They invited them to participate in what would be a one-hour event, featuring seven to 10 storytellers. Each person would have just five minutes to share a personal or patient-related experience around equity, diversity, and inclusion. The organizers did not want the same types of stories; they wanted a rich mix of perspectives. So, they asked anyone interested to send in a brief synopsis of their story.
As the event drew closer, the storytellers turned in their full stories. The organizing committee gave feedback, helped with editing, and worked with each storyteller to expand or tighten up certain aspects of their story to ensure that it could be told in the time limit. They offered encouragement and support to storytellers each step of the way leading up to the event.
The Night of the Event
On the night of the event, storytellers and audience members were excited. Although it was not required for any coursework or faculty duties, many members of the Division attended the event. Those attending in person were treated to a complimentary dinner. The event started with a warm welcome, followed by a description of three community agreements: (1) Respect the personal nature of the stories; while you might take away important lessons, the stories themselves are not to be retold; (2) There will be no questions or discussions after each story; the goal is to listen, not debate or build upon the stories; and (3) Be attentive and respectful because each storyteller is about to share something personal and vulnerable.
Then, one by one, the storytellers took the stage. Each was introduced by a member of the organizing committee who shared the storyteller’s name, role in the Division, and title of their story. After each storyteller recounted their five-minute story, the organizers displayed a meaningful quote, chosen by the storyteller, giving everyone a chance to reflect. Applause filled the room and for those attending virtually, the Zoom chat filled with messages of appreciation and support. When the final story was told, the organizers closed the evening. They thanked the storytellers for their courage and vulnerability and expressed gratitude to the audience for their presence and care for each story told. One story from the 2023 StorySlam is available here in the Appendix.
What Came After
Once the storytelling was done, the organizing committee sent out a survey to everyone who attended, asking about their experience. They included seven 5-point Likert scale questions, ranging from Strongly Disagree to Strongly Agree, to gauge how well the event had met the goal. Among the questions:
- Did people feel more connected to the community?
- Did they gain a deeper understanding of others’ experiences?
- Did the stories inspire them to participate in future events?
The survey also included two open-ended questions to give attendees a chance to share their thoughts more freely:
- What they loved about the event.
- What ideas they had for future StorySlams.
Two assessors (SJ and NDM) independently read the open-ended questions and responses to determine common themes. After they compared their findings, they worked together to resolve any differences and pulled out the key themes and the most insightful takeaways.
Results
The 2023 StorySlam event was attended by a total of 79 people, with 48 (60%) in-person and 31 (40%) remote attendees. Eight storytellers (four students, three faculty members, and one patient) shared their stories. The most common themes included: class/socioeconomics, belonging, and advocacy/social responsibility (Figure 1).
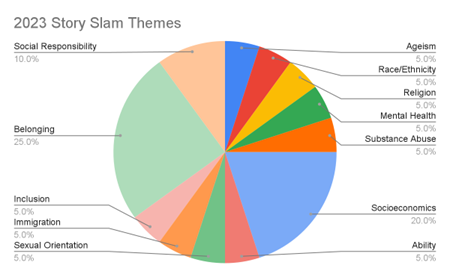
Figure 1: Themes identified in the stories presented in StorySlam 2023 along with their frequency of occurrence across stories.
The outcome survey received responses from 39 (49%) attendees, which included students, faculty, staff, and community members. Most attendees indicated agreement or strong agreement with the Likert scale items, with each item receiving an average score of greater than 4 out of 5 (Figure 2).
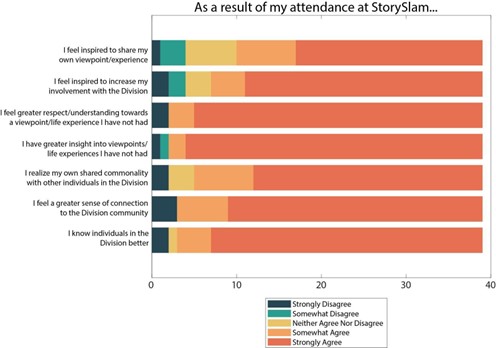
Figure 2: Responses to the StorySlam survey for the 2023 event. The questionnaire included seven items, shown on the y-axis here, each of which could be rated on a five-point scale ranging from “Strongly Disagree” to “Strongly Agree.” The length of each color bar represents the number of responses in that response category for that item. The total number of respondents was 38.
Among responders, 69% strongly agreed with the statement “I realize my own shared commonality with other individuals in the Division,” and 77% strongly agreed with the statement “I feel a greater sense of connection to the Division community.” Both of these factors can enhance an overall sense of belonging. A full 38 out of 39 (97%) respondents indicated that the event met their expectations.
Sample Responses
In the open-ended responses, several respondents appreciated that the storytellers spanned varied roles in the Division (students, faculty, patients), thereby allowing for a wide range of perspectives.
“I am really happy I went to listen and absorb my friends and teachers speak about their life experiences. It will help me grow as an individual and as a clinician.”
“Love the perspectives from faculty, students, community members – made this community feel richer.”
Others recognized and appreciated the strength and vulnerability required for people to tell their personal stories in front of a large group, with some attributing this to the safe space created in the room. Some respondents mentioned the event being an emotional experience for them, strengthening a feeling of community and inspiring them to tell their own stories in future events.
“I feel so grateful for being able to hear stories from our division and that of our community friends. I feel so inspired and motivated to do this next year and share my story.”
Some suggestions for this event in future years included improvement in audio quality for both in-person and online attendees, having the camera zoomed in on the speaker for those attending remotely, and increasing the frequency of this event with different themes such as love or clinical reflections.
Discussion
The StorySlam successfully provided opportunities for Division members to share and listen to a variety of stories, exposing members of our community to diverse perspectives and life experiences. There was an overwhelmingly positive response to the event, including an appreciation of the vulnerability of the storytellers and a sense that the community felt richer than participants had initially perceived. There were multiple suggestions for more events of this nature in the future.
Insights
Most of the stories in this StorySlam focused on socioeconomic class and belonging. Belonging has always been a consistent theme brought forward in the StorySlam, likely due to the prompt sent out in the invitation to share “a patient interaction, a cultural experience within the program, or a reflection that speaks to the theme of equity, diversity, and inclusion.” However, socioeconomic status had not been a common theme in the three StorySlams prior to 2023. This change could be attributed to the COVID-19 pandemic, which illustrated the disparities between how people of differing socioeconomic classes were impacted, as well as more recent concerns in society regarding the cost of college education and student loan burden after graduation. Stories that feel important to share may change over time and in different contexts, assisting us with understanding shifts in the profession and the wider culture, thereby expanding our perspectives.
The input we received from participants at this event is consistent with previous reports of the positive impact of storytelling on communities.7–9 Narrative medicine—the practice of medicine with empathy, reflection, professionalism, and trustworthiness—has long been championed as a way to improve a physician’s work with patients, other professionals, and the public.14 Although the StorySlam did not emphasize all aspects of narrative medicine, we intentionally paused between each story to give listeners time to reflect on what they heard and consider how elements of the story might challenge or reinforce their own perspectives. For some audience members, this reflection time may have allowed for empathy, resulting in attitude change and alliance building.15
Limitations
A limitation of the StorySlam is that participation of storytellers and audience members was voluntary and limited to students, educators, staff, and patients within one university’s Physical Therapy program. Additionally, the participants and audience members who chose to attend are likely those who already have an appreciation of the potential benefits of such an event. As such, the perspectives shared by this group may not be representative of the physical therapy academic and clinical community at large.
Finally, a limitation of our event survey was that it did not directly measure the event’s impact on attendees’ sense of belonging. Although two questions indirectly addressed belonging by asking about attendees’ feelings of connection and shared commonality within the Division, future surveys would benefit from including more direct questions and assessments of this construct.
Future Progress
In the future, we plan to continue hosting this annual event and will consider increasing the frequency to provide this platform to community members more often. This would provide more opportunities for those initially hesitant to share their stories to engage as well as provide more opportunities for reflection by the larger community. It may also be beneficial to provide storytelling platforms in other formats such as written stories or recorded audio stories.
Conclusion
In physical therapy practice and education, storytelling can build a strong sense of community and a supportive learning environment, where students, faculty, and staff are encouraged to share meaningful experiences with each other and learn from them. At our institution, a StorySlam has proved to be an impactful and realistic method to provide space for storytelling and achieve these benefits. These events can help facilitate an environment where diverse perspectives can be shared and reflections on these perspectives can deepen our understanding of ourselves, others, and our community.
Acknowledgment
The authors of this paper would like to thank Evan Harvey, PT, DPT for allowing us to share her story, Savior Syndrome and its Flaws, for our readers.
Appendix
Savior Syndrome and Its Flaws
By Evan Harvey
Told at the 2023 USC StorySlam. Printed with permission from the author.
In many of my rotations throughout inpatient acute and rehabilitation settings I have encountered a variety of patients with varied cultures, ideals, and economic backgrounds. One specific patient interaction that will stay with me forever involves a young man who had undergone a series of unfortunate issues that resulted in a long stay in the ICU and an even longer stay on the acute floor. This gentleman was houseless and going into the evaluation I was really encouraged to be able to provide him with support for his planned discharge. In short he had a lot of weakness, severe balance deficits, and was unsafe to ambulate independently. Immediately my mind went to a wheelchair for discharge based on patient presentation and my own clinical reasoning. Following the evaluation and discussion with the patient I told him “we are going to order you a wheelchair for discharge for your safety.” He responded with the following:
“If I were to have a wheelchair out on the street where I live it makes me a target for theft, violence, and more. I need to be able to navigate the streets without a device so no one thinks I am weak and tries to hurt me.”
I was shocked and feelings of guilt and sadness washed over me. At this point I didn’t know how to best help this patient. But I understood that I had made the assumption that I knew what was best for them. In the moment, I let my CI take over the interaction and continue the conversation with this individual. The gentleman discharged the next day with a front wheeled walker per recommendation and choice of the patient. During another rotation I had a whole year later working in acute care in both Inglewood and East Los Angeles, I ran into the same conversations with individuals.
This time I had the experience to be able to go into the conversation more confidently. I specifically remember a woman who had a CVA. Her time in the hospital was running short and while she desperately needed more therapy she opted for a self discharge and was determined to leave the hospital on her own. We sat down and had a conversation about her safety returning to living on Skid Row where her permanent residence was and how she could progress herself through exercises to optimize her function as she felt she wouldn’t be able to return to therapy after leaving the hospital.
I asked her what she felt was in her capacity to do and she stated she could not perform any exercises lying down on the ground as this made her a target for sexual assault; she rarely lay on the ground and usually slept upright in a chair because of this. Together we brainstormed exercises and progressions and created a large packet that she could keep with her and utilize over time. She felt confident in these interventions and was really happy and motivated to gain her strength back because she felt included in the process of her care.
These interactions absolutely changed my mindset regarding patient treatment and plan of care and how important it is to include patients and their support system in clinical decision making. At the end of the day, we have no idea all the things patients are facing until we sit down with them and take the time to better understand.
References
- Hammond JA, Williams A, Walker S, Norris M. Working hard to belong: a qualitative study exploring students from black, Asian and minority ethnic backgrounds experiences of pre-registration physiotherapy education. BMC Med Educ. 2019;19(1):372. doi:10.1186/s12909-019-1821-6
- Hwang IJ, Mancera CM, Ramirez RI, Woods RA, Bains M. Identifying the needs of a diverse cohort and engagement opportunities that foster a sense of belonging at a Hispanic-serving doctoral program. J Lat Educ. 0(0):1-13. doi:10.1080/15348431.2023.2271556
- Tobbell DA. Teaching with oral histories. Bull Hist Med. 2016;90(1):128-135.
- Peterson S. How stories help us see ourselves: the power of storytelling by physical therapists. Phys Ther. 2023;103(7):pzad046. doi:10.1093/ptj/pzad046
- Churchill LR, Churchill SW. Storytelling in medical arenas: the art of self-determination. Lit Med. 1982;1(1):74-81.
- Divinyi J. Storytelling: an enjoyable and effective therapeutic tool. Contemp Fam Ther. 1995;17(1):27-37. doi:10.1007/BF02249302
- Fivush R. The Power of Stories for Patients and Providers. J Humanit Rehabil. Available at: https://www.jhrehab.org/2017/10/17/the-power-of-stories-for-patients-and-providers/. Accessed January 11, 2025.
- Walsh A, Evans JE, Sims E, et al. Bedside audio storytelling for hospital patients: a program overview. J Humanit Rehabil. Available at: https://www.jhrehab.org/2017/10/17/bedside-audio-storytelling-for-hospital-patients-a-program-overview/. Accessed January 11, 2025.
- Greenfield BH, Jensen GM, Delany CM, Mostrom E, Knab M, Jampel A. Power and promise of narrative for advancing physical therapist education and practice. Phys Ther. 2015;95(6):924-933. doi:10.2522/ptj.20140085
- Ingram C. Storytelling in medical education, clinical care, and clinician well-being. Arch Med Health Sci. 2021;9(2):337. doi:10.4103/amhs.amhs_289_21
- Haigh C, Hardy P. Tell me a story — a conceptual exploration of storytelling in healthcare education. Nurse Educ Today. 2011;31(4):408-411. doi:10.1016/j.nedt.2010.08.001
- Kumagai AK, Wear D. “Making Strange”: a role for the humanities in medical education. Acad Med. 2014;89(7):973-977. doi:10.1097/ACM.0000000000000269
- Annals of Internal Medicine: Annals Story Slam. Annals of Internal Medicine. Available at: https://www.acpjournals.org/topic/web-exclusives/annals-story-slam. Accessed September 5, 2024.
- Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897-1902. doi:10.1001/jama.286.15.1897
- DeTurk S. Intercultural empathy: myth, competency, or possibility for alliance building? Commun Educ. 2001;50(4):374-384. doi:10.1080/03634520109379262















 Member since 2019 | JM14274
Member since 2019 | JM14274


NO COMMENT