Getting to the Heart of the Patient-Provider Interaction: A Novel Theoretical Framework
Table of Contents
Category: Method/Model Presentation
Compliance With Ethical Standards: The authors declare that they have no conflict of interest, and no affiliations with, or involvement in, any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript, and that no research was performed on any human or animal subjects that would require informed consent.
Abstract
BACKGROUND/PURPOSE: The inner workings of the patient-provider interaction (PPI) have been shown to have profound effects on patient outcomes and patient satisfaction. However, the interchangeable use of terminology such as “compassion” and “empathy” as well as the varying definitions of terms such as “rapport” or “therapeutic alliance” have made both teaching and applying these skills challenging. Thus, the purpose of this literature review is to synthesize the current data on the topic.
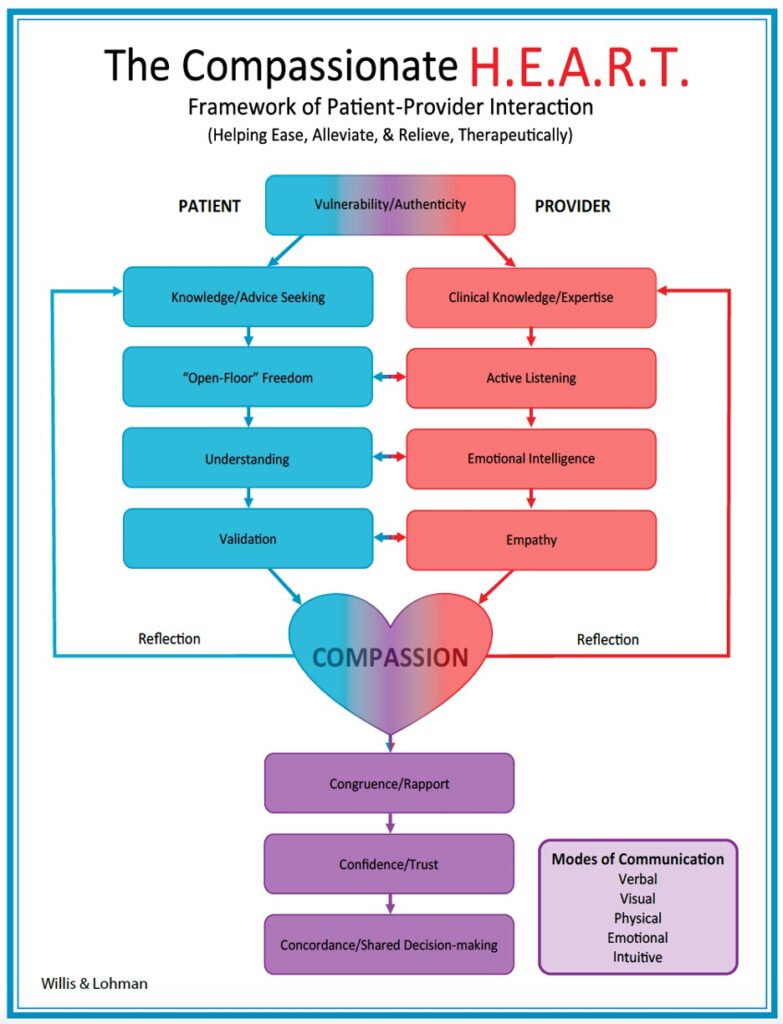
MODEL DESCRIPTION: A novel theoretical framework is introduced, which is intended to illustrate how each component relates, interacts with, and flows as the relationship between patient and healthcare provider progresses. Additionally, the new framework is proposed to provide improved clarity and enriched academic and clinical application of cultivating a successful PPI.
EVALUATION/OUTCOMES: The literature thus far illustrates the complexity of this relationship, warranting a more robust organization and approach to optimizing said relationship.
DISCUSSION/CONCLUSION: The Compassionate H.E.A.R.T. Model of Patient-Provider Interaction is a more thorough view of the dyadic PPI that is supported by the current literature. Further research is needed to evaluate both the academic and clinical application of the novel model.
Keywords: compassion; empathy, therapeutic alliance, patient-provider interaction, rapport[/vc_column_text][vc_column_text]
Introduction
“People don’t care how much you know until they know how much you care.”
–Theodore Roosevelt
This quote has been attributed to several different people over the years, but if its origins are from the lips of former president Theodore Roosevelt, then it would have first been uttered over a century ago, lending credence to the idea that caring should be well-ingrained into our collective consciousness, especially in the field of healthcare. However, a study conducted by Doohan and Saveman1 narrates a differing practice in the delivery of healthcare to patients. After a harrowing bus crash that claimed 6 lives, researchers interviewed the 56 survivors, 5 years following the crash. When asked about their memories of the event, they spoke of the physical pain, which is not surprising. The other factor that was cemented into their memories was a lack of compassion by caregivers at the hospital. What is even more disheartening is that they were all taken to multiple different hospitals.
While it may be argued that lack of compassion is an aberration in healthcare practice, the current body of literature paints a different picture. Thirteen-hundred patients and physicians were surveyed and asked if the U.S. healthcare system was compassionate; nearly half of them responded “no.”2 It appears that this disheartening trend continues; other more recent investigations reveal similar findings.3,4 The question then becomes, “Why?” While the answer is undoubtedly multifaceted, part of it likely lies in the education of healthcare professionals.3 It is well-established that compassionate care matters, as demonstrations of compassion have been shown to increase patients’ hope for recovery, accountability, control over their own health, satisfaction, safer care, happiness, and healthcare professional resilience—which leads to time and cost savings.4 Yet, there still exists a lack of clarity regarding the specifics of compassion in the administration of patient care.
In the literature on the topic of compassionate care, ambiguity appears regarding the terms compassion, empathy, caring, kindness, connection, rapport, and patient-provider relationship—terms that are often used synonymously—and makes merely collecting data challenging.5 In physical therapy, the most pervasive equivalent term used is “therapeutic alliance” (TA). A systematic review on the topic of TA defined it as having 3 components: 1) therapist-patient agreement on goals; 2) therapist-patient agreement on interventions; and 3) the affective bond between therapist and patient.6
Attempts by primary care physicians have also been made to illuminate how to create a sustained partnership with their patients, with the key components being: 1) whole-person focus; 2) physician’s knowledge of the patient; 3) caring and empathy; 4) patient trust of physician; 5) appropriately adapted care; and 6) patient participation in shared decision-making.7 However, these components are presented as free-standing concepts, with not much in the way of a flow that occurs in any encounter between 2 human beings, nor insights into how they interact with one another.
While any attempt at trying to quantify the dyadic nature of such a complex interaction will fall short of reality, this overly-reductionist view of a TA that is intended to attune ourselves to the phenomenological experience of our patients leaves a great deal to be desired. Combine that with the sheer confusion among terms used to describe the process, and it is apparent that a new approach to compassion in care is warranted.8
The Components of Compassionate Care
Thus, the purpose of this literature review is to introduce a novel theoretical framework to expound upon the complex nature of the patient-provider interaction (PPI), while simultaneously simplifying its application both in the classroom and the clinic. To address this purpose, first we will begin with a discussion of each component that goes into compassionate care, based on the literature, followed by the presentation of a novel framework.
Authenticity
There is agreement in the literature that vulnerability is a general human condition; it remains complex, multifaceted, and thus difficult to define.9 One of the complexities lies in how it is open to both objective and subjective definitions.10 Objectively, it can be defined as the interaction between capabilities and risks making up an individual’s wellness-illness status, yet subjectively, the person’s own assessment of this transaction is also part of the definition.11 Healthcare is already well-built to handle the objectively-defined vulnerabilities through its “calculative thinking” epistemology—or understanding of the world through scientific investigation.12 However, when someone has a certain aspect of their body seemingly “break down,” it is not only the body, but the life lived in that body, or, lived body, that is disturbed. There is a shift in the patient’s entire meaning-making process, leaving them to make sense of living in a body that now feels foreign.13 Whether the patient is aware of the subjective aspect of vulnerability or not, it is as equally important as the vulnerabilities that can be objectively measured and tested scientifically. This is true especially when one is attempting to connect with that person and their entire lived experience, as the meaning-making process that is disturbed by this subjective aspect of vulnerability drives their entire sense of being in their world.
Current medical practice’s focus on the scientific aspects of vulnerability often leads to an objectifying gaze from a distance, or a place of “detached concern,” that is detrimental to our ability to build a relationship.14 Healthcare providers must lean in and connect with our own vulnerabilities of our own lived experience in order to better enter the world of relationship.15 With the exploration of their own vulnerability, the healthcare provider triggers a shift toward authenticity, or a deepening of present being in the world that can operationally be described as a shift in attention and engagement and reclaiming of oneself from the way we typically fall into our everyday ways of being.12 The “default mode” of the human experience is shaped largely by the influence of others, often termed the “they,” as well as our own thoughts of who and what we think we should be. Just as the patient is forced to confront their vulnerability and loss of self/meaning, which forces them to face the facade they had put up in their inauthentic life as the “they,” it is the healthcare provider’s responsibility to enter this same space & confront our own mortality or potential to lose all that gives us meaning at any moment, which in turn also forces us to tear down the walls of our own inauthentic path. In other words, the provider must be able to fully exist authentically in the present moment, minimizing protective distancing from the suffering witnessed daily, in order to open themselves up to be able to enter a patient’s suffering. This is preferable rather than protectively shielding themselves from the anxieties associated with the vulnerability of their own humanness or that of those with whom they are attempting to build fellowship.13
Advice-Seeking and Clinical Knowledge/Expertise
Patients seek out healthcare providers for help. Whether a patient/provider visit targets mysteries surrounding bodily functions, healthier self-governance, or amelioration of pain, every patient is advice-seeking—in search of medically-informed guidance. Louis Gifford organized this fact when he proposed that every patient has 4 questions they are seeking to get answered: 1) What is wrong with me? 2) What can you do to help? 3) What can I do to help? and, 4) How long will it all take?16
PPIs offer unique opportunities for a healthcare provider who possesses extensive schooling, has undertaken rigorous clinical rotations, and has engaged in yearly continuing-education courses, to evaluate patients for unknown or unspecified pathologies and their related impairment and functional abilities. Accompanied by a desire to help others, practitioner competence (diagnostic as well as protocol efficacy) presents as a primary criterion in provider selection.17 In a systematic review of the literature on patient priorities for primary care, 19 studies found that the second most important factor in patient preference/provider selection was competency/accuracy, topped only by the quality of “humanness.” Humanness here is referred to as being viewed by the patient as “understanding, compassionate, attentive, treats you like an individual,” and is “patient, honest, friendly and pleasant, and sensitive to patients’ feelings.”17
This places a luminous spotlight on the importance of the “caring” in care provision. When a level of expertise/knowledge is combined with a genuine, caring desire to help, the genesis of optimal PPI becomes an achievable feat.
“Open-Floor” Freedom and Active Listening
One of the primary aspects of care that patients seek in a provider is the assurance that their views and preferences will be considered when devising a treatment plan.18 This serves as an important reminder that there are 3 key elements to Evidence-Based Practice (EBP): 1) Evidence; 2) Clinical expertise/expert opinion; and 3) Patient’s perspective.19 Patients must be provided an opportunity to share their views and preferences with their provider, secure in the knowledge that both are valued and utilized in formulation of treatment options. It is all too easy for well-meaning, busy clinicians to forget that the patient’s unique social, cultural, and personal circumstances as well as their values, expectations, beliefs, and priorities are critical elements to practicing evidence-based medicine (EBM).20 Unfortunately, the literature suggests healthcare providers fall short in this regard. On average, patients are interrupted while narrating their health concerns anywhere between 11 to 12 seconds21, 22 and 23 seconds.23 The clinician’s failure to listen fully is problematic because the patient is the biggest expert regarding their lived experience. Additionally, if patients are not allowed to actively participate in the conversation, it begs the question: how can any form of alliance be engineered to optimize care regimens?
A huge contributing factor to the above issue is the productivity standards inherent in healthcare systems. However, when given the opportunity to express themselves freely and uninterrupted at the start of a healthcare encounter, patients take an average of 92 seconds.24 It is vital to the patient and provider that the patient be able to share their thoughts, beliefs, and experiences freely in order to optimize patient care. Practitioners must thoughtfully and purposefully create “metaphoric space,” or allow an opportunity in the conversation for a “narrative discourse,” or communion in the form of “someone telling someone else that something happened.”25
The natural counterpart to someone having the space to speak their piece is active listening. Active listening is defined as a conscious processing of the stimuli being received through the auditory system via the passive process of hearing.26 Extensive literature published on this topic speaks to the vitality of this often-overlooked skill. Morgan et al27 highlighted how miscommunication occurring in PPIs is common and often proceeds undetected. The authors stated that “consultations are extremely complex interactional events, with numerous potential barriers to effective communication, including strict time constraints. It is therefore essential that general practitioners (GPs) work actively on strategies which minimize the risk of more serious communication problems occurring.”
Traeger et al28 compared intensive patient education to a placebo in patients with acute low back pain. The placebo in the study was active listening without offering information or advice. Placebo, Latin for “I will please,” is a procedure that is considered to have no therapeutic effect, designed merely to pacify and calm.29 Researchers concluded that adding 2 hours of patient education to first-line care did not improve low back pain outcomes as compared to the placebo intervention. Since both groups showed equal improvement, it could be argued that active listening is not a “sugar pill” but rather a viable and powerful tool.
Kaptchuck et al30 also relegated active listening to the placebo category, finding that: a “placebo” of enhanced therapeutic relationship consisting of a warm, friendly manner; active listening (such as repeating patient’s words, asking for clarifications); empathy (such as saying “I can understand how difficult Irritable Bowel Syndrome (IBS) must be for you”); 20 seconds of thoughtful silence while feeling the pulse or pondering the treatment plan; and communication of confidence and positive expectation (“I have had much positive experience treating IBS and look forward to demonstrating that acupuncture is a valuable treatment in this trial”); produced statistically- and clinically-significant effects on patient outcomes.
Similarly, Fuentes et al31 found that “enhanced therapeutic alliance,” measured as verbal behaviors, including active listening (ie, repeating the patient’s words, asking for clarifications); tone of voice; nonverbal behaviors (ie, eye contact, physical touch); and empathy (eg, “I can understand how difficult LBP must be for you”); appeared equally as important as Interferential Current (IFC) in pain modulation. From a mechanistic standpoint, it has been established that using patient-centered interview (PCI) skills such as active listening shows patients’ brain changes on functional resonance imaging (fMRI) related to decreased pain-related neural activation of the anterior insula.32 Haley et al33 concluded that active listening and self-awareness lead to improved empathy in healthcare providers and ultimately to improvements in quality of patient-centered care (PCC).
Understanding and Emotional Intelligence
From the patient’s perspective, the logical next step after having your space to share your story is to feel that your thoughts and feelings about that story are understood. It has been established that “failures in communication of information about illness and treatment are the most frequent source of patient dissatisfaction.”18 Researchers found that a high number of patients already have an idea about what is wrong and what may have caused their condition. But failing to articulate their experiential observations via open-floor freedom/active listening, or not having their thoughts and feelings about it properly understood are what contribute most to poor patient satisfaction and poor treatment outcomes. An examination of the literature reveals patients not only value “humanness” as the top quality they are seeking in a healthcare provider, but also that patients are looking for a provider willing to “explore patient needs” as well as “other aspects of relation & communication.”17
A key factor in ensuring the needs of another are being heard and understood is emotional intelligence (EQ)—having the ability to decode exactly what those needs are and how they are making the other person think or feel. This term was popularized by psychologist Daniel Goleman,34 in which he defines it as one’s ability to “recognize, understand, & manage their own emotions” as well as the ability to “recognize, understand, & manage the emotions of others.” Goleman goes on to dive deeper into EQ, elaborating on its 5 components: 1) Self-awareness; 2) self-regulation; 3) motivation; 4) empathy; and 5) social skills. For the purposes of this paper, EQ is defined as an examination of basic definitions of recognizing, understanding, and managing emotions in ourselves as well as in others.
When reviewing the literature on how EQ and its components relate to interactions between healthcare provider and patient, the message is clear: it plays a profound role. Miscommunication is a regularly-occurring phenomenon in healthcare interactions for many reasons.27 While mostly due to the complex nature of human communication, research seems to suggest that providers “cannot assume their communication has been successful or understood as intended,” implying that a certain degree of EQ is necessary to attempt to achieve that ever-elusive goal of understanding the thoughts, beliefs, or emotions that have been shared in the encounter.27 Without any exploration of thoughts and feelings regarding what is attempting to be communicated, there is no way to assess the level of understanding that has or has not been achieved. It has also been found that a physician’s EQ is positively correlated with patient self-rated satisfaction, and their level of trust in the physician, as well as their rating of the overall patient-doctor relationship (PDR).35 The literature has also demonstrated that using an emotional focus with empathic responses in order to understand the patient’s story (or, in other words, EQ) shows brain changes on fMRI related to decreased pain-related neural activation of the anterior insula.32
Validation and Empathy
Patients often seek healthcare for help with their pain experience; communication with those in pain is important, as the way that healthcare providers respond to patient sharing of pain-related stories has a significant impact on pain-related outcomes.36 Not only are patients seeking to be understood but also in search of validation, and how it is or is not provided to them in sharing their pain story.37 Linehan38 suggests that validation can best be defined as a legitimatization process where the listener communicates that the speaker’s thoughts and feelings are understandable and free from judgment. Based on this process, Linehan points out that validating a patient’s thoughts and feelings does not mean that the person validating necessarily agrees with the speaker’s perspective, but rather that the listener can simply understand why the patient thinks and feels as they do.39 While most clinicians might feel they already provide validation for their patients, the key factor is whether the patient feels validated by the listener’s response.40
The concept of validation is a vital step in the PPI. Countless patients—particularly those dealing with persistent pain—believe that others do not believe their pain story or, worse yet, doubt if their pain condition is legitimate.41 This issue not only rings true across cultures, but the difficulties are often amplified when the patient belongs to a culture or speaks a different language than the healthcare provider.42,43 In these instances, how support is offered is just as vital as what is communicated. The theory of psychological reactance suggests that individuals have a basic need for self-determination in affecting their own lives.44,45 The theory proposes that any messaging or persuasive attempt may constitute a threat to freedom and arouse reactance, which in turn leads to rejection of the message.46 This theory predicts that the more explicit and dominant a message is, the greater the perceived threat to freedom—and the psychological reactance it induces. This is countered by whether the message is deemed to have high “person-centered” qualities or is specifically intended to alleviate a distressed person’s emotional state.47 Research has centered primarily on marital relationships. However, a clear correlation exists between the level of perceived person-centeredness of a response and principles of psychological reactance, which can be applied to the PPI.48 Thus, it is imperative that the provider’s message of validation be paired with genuine empathy to attempt to mitigate any psychological reactance.
Empathy is a widely-discussed topic that often leads to varying definitions and components regarding what it entails. In addition, empathy is a topic that is layered, rather than presenting as a single observable trait. Riess49 described empathy as “a human capacity that is best understood as several facets that work together to enable us to be moved by the plights and emotions of others.” Riess elaborates by stating, “our empathic capacity requires specialized brain circuits that allow us to perceive, process, and respond to others.” Thus, it is the combination of these 3 activities (perceiving, processing, and responding) that allows someone to show empathy.
For example, a provider demonstrating empathy as just described would be able to perceive that their patient is frustrated by not feeling heard, and process that information to effectively respond by allowing them the time and space to share their experience. While overlap exists between EQ (as defined above), empathy (as defined here), and compassion (defined in the next section), the goal of this manuscript is to attempt to sort out the subtle differences without being heavily reductionist. The perception occurs first with EQ, followed by empathy as the processing, interpretation, and relating to those perceptions, and involves both cognitive and emotional intelligence, among other components of empathy whose definitions are beyond the scope of this article.
As for the relevance of empathy in the PPI, the evidence is potent. In a large cohort study investigating over 240 Italian physicians and nearly 21,000 patients with diabetes, it was found that the patients of physicians who scored low on self-rated empathy had a 41% greater risk of diabetic complications.50 Analogous findings were also seen with a smaller, but still significant sample size in the United States as well. A study of almost 900 patients under the care of nearly 30 physicians found that there was a 16% difference between the A1C hemoglobin testing as well as a 15% difference in low-density lipids (LDL) cholesterol levels of diabetic patients in favor of the high-rating empathy physicians.50 Similar findings were seen when investigating disability among migraine sufferers and their assessment of their physician’s level of empathy. The patients of physicians with higher patient-rated empathy scores showed statistically- and clinically-significant improvement in compliance with diet/meal timing, exercising, stress modulation activities, sleep modification, medication use, and overall patient outcomes.52
In another example, a large prospective study of the placebo effect found that when placebo acupuncture was paired with an “augmented” patient-provider relationship (consisting of warmth, attention, active listening, and empathy), the intervention had similar effects as those seen in clinical trials of drugs currently used to treat irritable bowel syndrome.30 Looking into the trauma surgical ward of the hospital, a place where technical medical skills are classically thought to be the dominant factor regarding patient outcomes, we see more of the same results. Patient-reported assessment of physician empathy was the strongest predictor of treatment outcome at both 6 weeks (short-term outcomes) and 12 months (long-term outcomes) following patient discharge.53 As alluded to earlier, there is a final step in an empathic response, and that is the actual response or action, which we have defined as compassion.
Compassion
The concept of compassion is esoteric even when being investigated via scientific inquiry. A widely-agreed-upon definition could not be ascertained from the available literature. In its simplest form, compassion can broadly be described as “a concern for the well-being of others.”54 However, given the overlaps covered above, a more succinct definition could be helpful to further distinguish compassion from its other close relatives.
Compassion has been further defined as “a multi-textured response to pain, sorrow and anguish that includes kindness, empathy, generosity, and acceptance, with the strands of courage, tolerance, and equanimity equally woven into its cloth.”55 Elaborating further, the authors state that compassion is “the capacity to be open to the reality of suffering and to aspire to its healing.” While this definition offers slightly more clarity on what exactly compassion is, there is still some ambiguity.
Goetz et al56 provide further elements of the broader definition including “the feeling that arises in witnessing another’s suffering and that motivates a subsequent desire to help.” This definition paints compassion as an affective state in response to a subjective feeling, rather than an attitude. If compassion is often quoted as being “empathy in action,”57 the desire to help paired with subsequent action is the differentiating factor between compassion and empathy. For the purposes of this article, the following 4 components of compassion and the foundation for this framework include: 1) awareness of suffering (cognitive/empathic awareness); 2) sympathetic concern related to being emotionally moved by suffering (affective component); 3) a wish to see the relief of that suffering (intention); and 4) a responsiveness or readiness to help relieve that suffering (motivational).58
Research that investigated compassion and its effect on patient-provider interactions is limited in scope and purview. In fact, this dearth of available literature was motivational in the creation of our theoretical model. Additionally, as the title of the model (Compassionate H.E.A.R.T. Model) suggests, it is this understanding with an intention to help.” A clear overlap exists between that definition and what we defined as compassion above. Which factor was measured and how did they both influence the results? Similar questions arise with nearly all the studies focused on empathy. Some researchers52,53 used the Consultation and Relational Empathy (C.A.R.E.) Measure. Despite having empathy in the title of the outcome measure, another study used the same C.A.R.E. measure and found that compassion is correlated with decreased incidence of post-traumatic stress disorder (PTSD) in emergency room patients.59 When reviewing questions that appear on the C.A.R.E. Measure, one explicitly asks about the provider’s level of “care and compassion,” which adds to the confusion regarding distinguishing compassion from empathy. It is unclear if one factor was more influential than the other on outcomes achieved related to patient compliance and treatment outcome.
The researchers of this theoretical framework are not alone in questioning this overlap between the terms. In a recent prospective cohort study60 of almost 6,500 patients and their outpatient physicians, a tool to measure clinical compassion was developed and was shown to have strong internal consistency and convergent validity to identify the patient’s experience related to compassion or compassionate care. That same tool was utilized in a cross-sectional investigation61 of nearly 900 patients and their emergency room physicians. Results revealed excellent reliability and an ability to assess patient experience (compassion), distinct from mere patient satisfaction.
Despite lack of research on the direct effect of compassion on PPIs, the transition from empathy to compassion is vital to managing the cost of care62 and is thought to function in a stress-buffering manner for the clinician,54 with significant implications for a medical system riddled with clinician burnout. Clearly, all seem to play a pivotal role in the process of PPIs leading to successful patient health outcomes, which highlights the importance of distinguishing the components that contribute to a successful interaction.
Congruence/Rapport
Rapport is described as “a friendly relationship in which people understand each other well.”63 Congruence, or “genuineness,” is “an aspect of the therapy relationship with two facets, one intrapersonal and one interpersonal.”64 Mindful genuineness, personal awareness, and authenticity characterize the intrapersonal element. The capacity to give voice respectfully and transparently to one’s experience to another person characterizes the interpersonal component. Congruence, then, occurs when rapport meets the intersectionality of integrity during an interaction with another.
Integrity cannot occur without rapport. However, rapport can happen without congruence, which is most easily visualized with the example of the “sleazy used car salesman,” who is establishing an artificial connection simply for the sake of making a sale. Essentially, the goal of this phase of the therapeutic relationship is to establish rapport in conjunction with congruence, internally with oneself, and externally with the patient. To continue down the path in unison, the patient and practitioner must demonstrate a genuine and honest understanding of one another.
Progressing through the proposed theoretical framework, a poverty of quality research exists with which to support each section that contributed to the focused development of the framework itself, while also providing structure for future research on investigation of the PPI. For congruence specifically, the only significant literature on the topic has been published within the field of psychology. A recent meta-analysis65 found congruence to be a noteworthy factor that positively influenced patient outcomes, but with reservations due to the limited number of recent studies looking into congruence’s association with outcomes, the absence of any randomized controlled trials, and the small range of effect sizes in newer studies.
Rapport, on the other hand, has been investigated via works that have explored TA. A strong TA has been shown to be positively associated with: 1) treatment adherence in patients with brain injury and patients with multiple pathologies seeking physical therapy; 2) a reduction in depressive symptoms in patients with cardiac conditions and those with brain injury; (3) treatment satisfaction in patients with musculoskeletal conditions; and (4) improved physical function in geriatric patients and those with chronic low back pain.6
Confidence/Trust
Trust is defined as “assured reliance on the character, strength, ability, or truth of someone or something.”66 According to developmental psychologist Erik Erikson, the theoretical battle of trust vs. mistrust is the very first state of psychosocial development, occurring during the first 2 years of life.67 This sense of trust or mistrust is learned by the child through their interactions with their environment during this critical developmental stage. Similarly, in the PPI framework, the same concept is developed in both the patient and the provider while progressing through each stage. Once established in both directions, this leads to confidence, or the “faith or belief that one will act in a right, proper, or effective way.”68 This confidence is fostered via the means of trust. Without trust developed throughout the previous stages of interaction, confidence in the shared decision-making in the next step is omitted.
While the literature is sparse, the importance of confidence and trust in PPIs is somewhat intuitive. In a retrospective study69 of audiotaped interactions with Gulf War veterans, it was found that engagement and trust were positively associated between the patient and provider, as well as the only 2 patient factors that were associated with patient-provider concordance or working collaboration. In studies where the definition of TA was previously described as extremely broad, including “the affective bond between patient and therapist,” it can be argued that a portion of the positive effects on treatment adherence, depressive symptoms, treatment satisfaction, and physical function can be attributed, at least in part, to confidence and trust.6
Concordance/Shared Decision-Making
Concordance refers to the patient and the provider listening to one another’s thoughts and beliefs about the issue, negotiating a shared understanding of those beliefs, and coming to an agreement about how to move forward.70 Concordance is commonly referred to as “shared decision-making” about both problem and intervention, which is the core of the popular buzz-phrase “patient-centered communication,”71 and the end goal of this novel theoretical framework.
Patients have made it clear they want and value a role in the decision-making process.17, 18, 35, 69 For most practicing clinicians, the paternal biomedical model is still preferred, which likely contributes to lack of data informed by the patient perspective. It is possible that missteps in the proposed process of navigating the PPI also contribute to interactions failing to reach this critical stage.
Modes Of Communication
While we have outlined an understanding of each of the components of our novel framework, it is of paramount importance to also acknowledge the modes of communication through which each of these is being communicated between patient and provider. No exchange between 2 people can occur without a vehicle of transfer. Communication, defined as “a process by which information is exchanged between individuals through a common system of symbols, signs, or behaviors,”72 is an integral piece of any medical encounter. However, miscommunications are a frequent and complex phenomenon.27 This systematic framework that accounts for all of the modes of communication taking place during the exchange of information between a patient and their healthcare provider could provide insights into better grasping how to resolve this issue.
Verbal communication is probably the most researched of all the mechanisms of communication. It is well-established that words have the power to heal;73 however, healing is often attributed to the placebo effect. Similarly, words have the power to have a negative effect seen in patients given a “brief negative verbal suggestion on how previous studies have shown that exercise can induce pain,”74 commonly referred to as a “nocebo effect.” Practitioners must be aware of how varying forms of communication contribute to health outcomes,75 particularly when attempting to avoid iatrogenic ailments, or instances where “doctors [along with their words, thoughts, beliefs, feelings, and actions], drugs, diagnostics, hospitals, and other medical institutions act as ‘pathogens’ or ‘sickening agents.’”76 The bottom line is that words matter and can either harm or heal; thus, we must be mindful of them.
Although verbal tends to be the dominant form of communication, a large portion of the information exchange in a healthcare interaction is nonverbal.77,78 Specific to visual communication, behaviors such as a lack of smiling, nodding, or making eye contact have been shown to have a negative effect on both the physical and cognitive function of inpatient geriatric patients, after controlling for the patient’s physical and cognitive function at the time of admission. Inverse findings also held true for positive visual cues (eg, smiling, nodding, making eye contact, etc.) in improving function.79
Human touch is another powerful means of communication that has been shown to have a positive effect on the healing of patients in various settings.80 These effects aren’t limited to the “skilled touch” of manual interventions, but also through the means of transferring a caring energy of connection through “therapeutic touch.”81 Similarly, communicating via shared emotions has also been shown to have a positive effect on healthcare interactions.30, 31 Space has also been saved for communication deemed intuitive in nature, or, similar to placebo effect—potential means by which we have yet to understand.82
Mindful use of available means of communication moves the practitioner from section to section of the sequenced algorithm with iterative loop (theoretical framework), ideally ending at the intended outcome of a positive PPI and development of a concordant plan to address patient concerns.
The Compassionate H.E.A.R.T Model
Putting all the above evidence together, we arrive at the proposed Compassionate H.E.A.R.T. (Helping Ease, Alleviate, & Relieve Therapeutically) Model (Figure). It was developed by the authors to provide a structured framework for teaching and clinical application of this approach to the PPI.
FIGURE 1
Model Description
As shown in this model, the starting point for both parties is vulnerability and authenticity. The patient is inherently vulnerable in their wrestle with some form of illness and seeking care for the objective and subjective aspects of that vulnerability. The provider must step into the patient’s suffering by confronting their own human vulnerability—thus liberating both parties to authentically be in the moment and establish a connection of lived experience.
With that first step established, the model segues by appreciating the intersect of 2 separate lived experiences by the provider and patient that is inherent to the start of any healthcare interaction. The patient comes to a practitioner seeking some sort of knowledge or advice based on the clinical expertise that the provider possesses. The patient is often seeking an opportunity to tell their story, without interruption (open-floor freedom), while the provider is actively listening. Ideally, if the provider can attune to cues on what the patient is feeling regarding their thoughts, beliefs, feelings, and experience (emotional intelligence), a level of understanding may be achieved.
The provider’s empathetic ability to relate to the patient’s thoughts, beliefs, feelings without judgment is then paired with validation for the patient and their lived experience. It is this feeling of having someone else come alongside of the patient to validate their experience as real, combined with the provider’s internal “at oneness” with the patient resulting from “crossing over” into their lived experience and getting themselves back,83 that is hypothesized by the authors to lead to a transformation in the interaction—a dyad forming a singular unit, working together toward a solution. This key shift in the relationship occurs when both parties arrive at compassion; or empathic desire to help, hence why this sentiment compassion sits at the figurative and literal heart of the model.
Once arriving at this key transformational stage of compassion, the relationship then continues to shape a level of congruence, in the form of a mutual respect for each other’s role in the working relationship (rapport). With this newfound understanding, the interaction moves forward into a place of confidence that is achieved via a means of trust, until finally arriving at a place of concordance, or shared decision-making regarding the proper path to take to reach the mutually-agreed-upon goals.
Reflection
Realistically, each step of the interaction will not always flow smoothly. Clinician and patient interactions can at times be messy. To account for this, a vital component of the model is ongoing reflection, meaning the opportunity for each party to step back and analyze how the relationship is processing through the stages, potentially retreating to a previous step to ensure that every step is properly executed.
Reflection can transpire anywhere along the process but is shown midway (Figure) for purposes of simplicity. This reflective process, defined as “critical and conscious thought about one’s behavior and practice”84 or as a careful exploration and evaluation of experience,85 is paramount for any attempts to “bridge the divide” that separates provider from patient via what is known as “narrative competence,” or the “ability to absorb, interpret, and act on the stories and plights of others.”26 Within the act of reflecting on the interaction in real time as well as in retrospect lies the ability to foster the kinship between the patient’s lived experience and that of the provider’s as well, thus creating the medical care that is desired by both parties.
Modes of Communication
Lastly, the model accounts for how all stages are communicated between both parties throughout the process. Modes of communication include:
- Words and sounds that are uttered verbally;
- Non-verbal communication that is taken in visually;
- Any physical forms of communication such as touch;
- Emotions that are exchanged, which are often expressed via a mix of the other forms of communication; and lastly,
- Holding space for the intuitive nature of communication between 2 human beings.
Discussion/Conclusion
The information presented in this article is not necessarily groundbreaking. As evidenced by the references, a plethora of attempts have been made to understand the PPI. However, deficits still exist in the literature in terms of assimilating the information in a manner that aids in transforming it into something truly teachable. Historically, the topics discussed here have been treated as “the art of medicine” or “soft skills” that cannot necessarily be objectively taught nor measured, while the core knowledge has been the “science.” The deeper that we collectively dive into the intricacies of the PPI, the more evident it is becoming that these concepts of “art” and “science” are inseparable when discussing the lived human experience. True, there is an art to clinical practice. But the goal of this framework and future works focusing on it is to help show that there is indeed science woven within this art, as well as art intertwined within the science. Thus, a topic such as the PPI needed a framework to facilitate its instruction to both current and future healthcare providers, as structure provides the foundation for creativity, or “the art,” to flourish.
The novel theoretical framework presented here is intended to do just that: to organize the information in a manner that allows it to be standardized across all disciplines. As with the creation of any algorithm, we are cognizant of the line between being reductionist and attempting to simplify the complex nature of helping those in need into some form of “rubric” that can be graded. That is not the intent here, as so much of connecting on a human level is impossible to simplify or turn into a “science” to some degree. Or, to put it more articulately, “the body that one experiences cannot be reduced to the body that someone else measures.”13 So much of the key to improving this facet of medicine exists in the hypothetical margins of our collective “humanness.” That is, developing the vulnerability that acts as the key to unlocking this entire process, as well as incorporating more reflection, not only on this process, but more instances of bringing the humanities into its education using stories and the arts that describe the changes seen in our patients’ lived experiences. The future might even paint a different picture of all the components at play here.
A logical next question would be to ask what the application of this framework looks like in the classroom and in the clinic, as well as if the framework seems to make a difference in terms of outcomes for our patients. Plans specific to the authors are already in the works to explore the clinical effectiveness of approaching the PPI under this lens, as well as outlining what the application would look like in a case scenario. The robustness of the literature review here led the authors to believe both would likely be better suited for forthcoming works. The goal here was to introduce the framework and supporting literature to serve as a launching pad for future research, for improving instruction, and for simplifying clinical practice, while still honoring the complexity of 2 lived experiences intersecting.
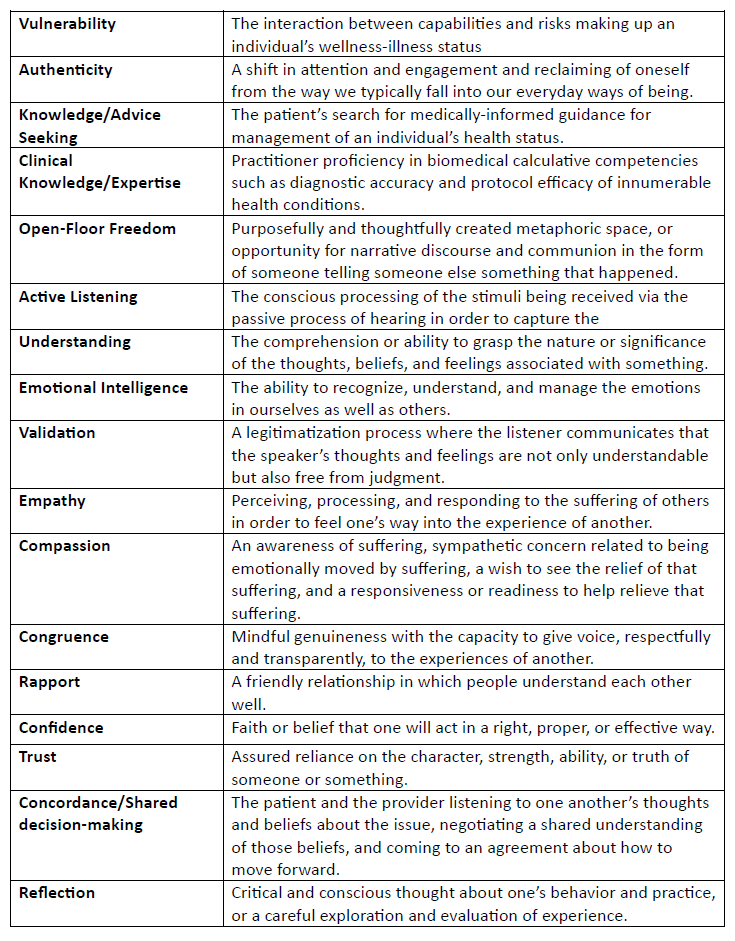
FIGURE 2
The Compassionate H.E.A.R.T. Model Operational Definition of Terms
References
- Doohan I, Saveman BI. Need for compassion in prehospital and emergency care: a qualitative study on bus crash survivors’ experiences. Int Emerg Nurs. 2015;23(2):115–119. https://doi.org/10.1016/j.ienj.2014.08.008
- Lown BA, Rosen J, Marttila J. An agenda for improving compassionate care: a survey shows about half of patients say such care is missing. Health Affairs (Project Hope). 2011;30(9):1772–1778. https://doi.org/10.1377/hlthaff.2011.0539
- Sinclair S, Russell LB, Hack TF, et al. Measuring compassion in healthcare: a comprehensive and critical review. 2017;10:389–405.
- Tehranineshat B, Rakhshan M, Torabizadeh C, Fararouei M. Compassionate care in healthcare systems: a systematic review. JAMA. 2019;111(5):546–554. https://doi.org/10.1016/j.jnma.2019.04.002
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331(7524);1064–1065. https://doi.org/10.1136/bmj.38636.593461.68
- Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90(8):1099–1110. https://doi.org/10.2522/ptj.20090245
- Leopold N, Cooper J, Clancy C. Sustained partnership in primary care. J Fam Pract. 1996;42(2):129-137.
- Trzeciak S, Booker C, Mazzarelli A. Compassionomics: The Revolutionary Scientific Evidence That Caring Makes A Difference. Studer Group. 2019. https://www.compassionomics.com/
- Angel S, Vatne S. Vulnerability in patients and nurses and the mutual vulnerability in the patient-nurse relationship. J Clin Nurs. 2017;26(9-10):428–1437. https://doi.org/10.1111/jocn.13583
- Gjengedal E, Ekra EM, Hol H, Kjelsvik M, Lykkeslet E, Michaelsen R, et al. Vulnerability in health care: reflections on encounters in everyday practice. Nurs Phil. 2013;14(2):127–138. https://doi.org/10.1111/j.1466-769x.2012.00558.x
- Sellman D. Towards an understanding of nursing as a response to human vulnerability. Nurs Phil. 2005;6(1):2–10. https://doi.org/10.1111/j.1466-769x.2004.00202.x
- Heidegger M. Memorial address. In: Anderson J, Freund EH, (trans). Discourse on Thinking. Harper & Row; 1969.
- Piemonte NM. Afflicted: How Vulnerability Can Heal Medical Education and Practice. MIT Press; 2018.
- Halpern J. From Detached Concern to Empathy: Humanizing Medical Practice. Oxford U Press; 2001. https://doi.org/10.1093/acprof:osobl/9780195111194.001.0001
- Nordstrom TM. Developing habits of the heart: 22nd Polly Cerasoli Lecture. J Phys Ther Educ. 2019;33(4):259–272. https://doi.org/10.1097/jte.0000000000000133
- Gifford L. Aches and Pains. Falmouth: CNS; 2014.
- Wensing M, Jung HP, Mainz J, Olesen F, Grol R. A systematic review of the literature on patient priorities for general practice care. Part 1: description of the research domain. Social Sci Med. 1982;7(10):1573–1588. https://doi.org/10.1016/s0277-9536(98)00222-6
- Coulter A. What do patients and the public want from primary care?. BMJ. 2005;331(7526):1199–1201. https://doi.org/10.1136/bmj.331.7526.1199
- Zadro J, O’Keeffe M, Maher C. Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open. 2019;9:e032329. doi:10.1136/bmjopen-2019-032329
- Meira E. Understanding evidence-based medicine using a funnel analogy. Research Gate. 12/10/2020. https://doi.org/10.31236/osf.io/kr6aq.
- Rhoades DR, McFarland KF, Finch WH, Johnson AO. Speaking and interruptions during primary care office visits. Family Med. 2001;33(7):528–532.
- Singh Ospina N, Phillips KA, Rodriguez-Gutierrez R, Castaneda-Guarderas A, Gionfriddo MR, Branda ME, et al. Eliciting the patient’s agenda: secondary analysis of recorded clinical encounters. J Gen Int Med. 2018;34(1):36–40. https://doi.org/10.1007/s11606-018-4540-5
- Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient’s agenda: have we improved? JAMA. 1999;281(3):283–287. https://doi.org/10.1001/jama.281.3.283
- Langewitz W, Denz M, Keller A, Kiss A, Rüttimann S, Wössmer, B. Spontaneous talking time at start of consultation in outpatient clinic: cohort study. BMJ. 2002;325(7366):682–683. https://doi.org/10.1136/bmj.325.7366.682
- West R, Turner LH. Understanding Interpersonal Communication. (2nd ed.). Cengage Learning; 2010.
- Charon R. The patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897–1902. https://doi.org/10.1001/jama.286.15.1897
- Morgan S. Miscommunication between patients and general practitioners: implications for clinical practice. J Prim Health Care. 2013;5(2):123–128.
- Traeger AC, Lee H, Hübscher M, Skinner IW, Moseley GL, Nicholas, MK, et al. Effect of intensive patient education vs placebo patient education on outcomes in patients with acute low back pain: a randomized clinical trial. JAMA Neurology. 2019;76(2): 161–169. https://doi.org/10.1001/jamaneurol.2018.3376
- Placebo. (n.d.). Available at: https://www.oxfordlearnersdictionaries.com/definition/english/placebo?q=placebo. Accessed 5/08/21/
- Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008; 336(7651): 999–1003. https://doi.org/10.1136/bmj.39524.439618.25
- Fuentes J, Armijo-Olivo S, Funabashi M, Miciak M, Dick B, Warren S, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2014;94(4):477–489. https://doi.org/10.2522/ptj.20130118
- Sarinopoulos I, Hesson AM, Gordon C, Lee SA, Wang L, Dwamena F, et al. Patient-centered interviewing is associated with decreased responses to painful stimuli: an initial MRI study. Patient educ Couns. 2013;90(2):220–225. https://doi.org/10.1016/j.pec.2012.10.021
- Haley B, Heo S, Wright P, Barone C, Rao Rettiganti M, Anders M. Relationships among active listening, self-awareness, empathy, and patient-centered care in associate and baccalaureate degree nursing students. NursingPlus Open. 2017;3:11-16. doi:10.1016/j.npls.2017.05.001
- Goleman D. Emotional intelligence: why it can matter more than IQ. Bloomsbury; 1996.
- Weng HC, Chen HC, Chen HJ, Lu K, Hung SY. Doctors’ emotional intelligence and the patient-doctor relationship. Med Educ. 2008;42(7):703–711. https://doi.org/10.1111/j.1365-2923.2008.03039.x
- Hadjistavropoulos T, Craig KD, Duck S, Cano A, Goubert L, Jackson P, et al. A biopsychosocial formulation of pain communication. Psych Bulletin. 2011;137(6):910–939. https://doi.org/10.1037/a0023876
- Cano A, de C Williams AC. Social interaction in pain: reinforcing pain behaviors or building intimacy? Pain. 2010;149(1):9–11. https://doi.org/10.1016/j.pain.2009.10.010
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; 1993.
- Linehan M. Validation and psychotherapy. In: Bohart A, Greenberg LS, eds. Empathy reconsidered: New directions in psychotherapy. Washington DC: American Psychological Association; 1997.
- Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–219. https://doi.org/10.1097/01.j.pain.0000460301.18207.c2
- Kool MB, van Middendorp H, Boeije HR, Geenen R. Understanding the lack of understanding: invalidation from the perspective of the patient with fibromyalgia. Arthritis Rheum. 2009;61(12):1650–1656. https://doi.org/10.1002/art.24922
- Narayan MC. Culture’s effects on pain assessment and management. Am J Nurs. 2010;110(4):38–49. https://doi.org/10.1097/01.NAJ.0000370157.33223.6d
- Krupić F, Čustović S, Jašarević M, Šadić S, Fazlić M, Grbic, K, et al. Ethnic differences in the perception of pain: a systematic review of qualitative and quantitative research. Medicinski Glasnik. 2019;16(1):108–114. https://doi.org/10.17392/966-19
- Brehm JW. A Theory of Psychological Reactance. Academic Press; 1966.
- Brehm SS, Brehm JW. Psychological Reactance: A Theory of Freedom and Control. Academic Press; 1981.
- Dillard JP, Shen L. On the nature of reactance and its role in persuasive health communication. Commun Monographs. 2005;72(2):144–168. https://doi.org/10.1080/03637750500111815
- Feng B, Burleson BR. The effects of argument explicitness on responses to advice in supportive interactions. Commun Res. 2008;35:849–874. doi:10.1177/0093650208324274.
- Xi T, Haunani S, St. Cyr B. How the comforting process fails: psychological reactance to support messages. J Commun. 2020;70(1):13–34. https://doi.org/10.1093/joc/jqz040
- Riess H, Neporent L, Alda A. The Empathy Effect: Seven Neuroscience-Based Keys For Transforming The Way We Live, Love, Work, And Connect Across Differences. Boulder, CO: Sounds True; 2018.
- Del Canale S, Louis DZ, Maio V, Wang X, Rossi G, Hojat M, et al. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. J Assoc Am Med Coll. 2012;87(9):1243–1249. https://doi.org/10.1097/ACM.0b013e3182628fbf
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. J Assoc Am Med Coll. 2011;86(3):359–364. https://doi.org/10.1097/ACM.0b013e3182086fe1
- Attar HS, Chandramani S. Impact of physician empathy on migraine disability and migraineur compliance. Ann Ind Acad Neuro. 2012;15(Suppl 1):S89–S94. https://doi.org/10.4103/0972-2327.100025
- Steinhausen S, Ommen O, Antoine SL, Koehler T, Pfaff H, Neugebauer E. Short- and long-term subjective medical treatment outcome of trauma surgery patients: the importance of physician empathy. Patient Pref Adhere. 2014;8:1239–1253. https://doi.org/10.2147/PPA.S62925
- Cosley B, McCoy S, Saslow S. Is compassion for others stress buffering? Consequences of compassion and social support for physiological reactivity to stress. J Exp Soc Psych. 2010;46(5):816-823.
- Feldman C, Kuyken W. Compassion in the landscape of suffering. Contemp Buddhism. 2011;12(1):143-155. doi:10.1080/14639947.2011.564831.
- Goetz JL, Keltner D, Simon-Thomas E. Compassion: an evolutionary analysis and empirical review. Psych Bulletin. 2010;136(3):351–374. https://doi.org/10.1037/a0018807
- Jinpa T. A Fearless Heart: Why Compassion Is The Key To Greater Wellbeing. Piatkus; 2017.
- Jazaieri H, Jinpa GT, McGonigal K. et al. Enhancing compassion: a randomized controlled trial of a compassion cultivation training program. J Happiness Stud. 2013;14:1113–1126. https://doi.org/10.1007/s10902-012-9373-z
- Moss J, Roberts MB, Shea L, Jones CW, Kilgannon H, Edmondson DE, et al. Healthcare provider compassion is associated with lower PTSD symptoms among patients with life-threatening medical emergencies: a prospective cohort study. Intens Care Med. 2019;45(6):815–822. https://doi.org/10.1007/s00134-019-05601-5
- Roberts BW, Roberts MB, Yao J, Bosire J, Mazzarelli A, Trzeciak S. Development and validation of a tool to measure patient assessment of clinical compassion. JAMA. 2019;2(5):e193976. https://doi.org/10.1001/jamanetworkopen.2019.3976
- Sabapathi P, Roberts MB, Fuller BM, Puskarich MA, Jones CW, Kilgannon JH, et al. Validation of a 5-item tool to measure patient assessment of clinician compassion in the emergency department. BMC Emerg Med. 2019;19(1):63. https://doi.org/10.1186/s12873-019-0279-5
- Brown SL, Brown RM. Connecting prosocial behavior to improved physical health: contributions from the neurobiology of parenting. Neurosci Biobehav Rev. 2015;55:1–17. https://doi.org/10.1016/j.neubiorev.2015.04.004
- Rapport. (n.d.) Available at: https://www.oxfordlearnersdictionaries.com/us/definition/english/rapport. Accessed May 10, 2021.
- Rogers CR. The necessary and sufficient conditions of therapeutic personality change. J Consult Psych. 1957;21:95–103. http://dx.doi.org/10.1037/h0045357
- Kolden GG, Wang CC, Austin SB, Chang Y, Klein MH. Congruence/genuineness: a meta-analysis. Psychother. 2018;55(4):424–433. https://doi.org/10.1037/pst0000162
- Trust. (n.d.) Available at: https://www.merriam-webster.com/dictionary/trust. Accessed May 10, 2021.
- Kalat JW. Introduction to Psychology. Thomson Wadsworth; 2010.
- Confidence. (n.d.) Available at: https://www.merriam-webster.com/dictionary/confidence. Accessed May 10, 2021,
- Friedlander ML, Kangos KA, Maestro KJ. Introducing an observational rating system for studying concordance in patient–physician relationships. Counsel Psych. 2019;5:796-819. doi:10.1177/0011000019891434
- Royal Pharmaceutical Society of Great Britain From Compliance To Concordance: Achieving Shared Goals In Medicine Taking. London, England: Royal Pharmaceutical Society; 1997.
- Epstein RM, Franks P, Fiscella K, Shields CG, Meldrum SC, Kravitz RL, et al. Measuring patient-centered communication inpatient–physician consultations: Theoretical and practical issues. Soc Sci Med. 2005; 61:1516–1528. doi:10.1016/j.socscimed.2005.02.001
- Communication. (n.d.) Available at: https://www.merriam-webster.com/dictionary/communication. Accessed May 10, 2021,
- Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Counsel. 2009;74(3):295–301. https://doi.org/10.1016/j.pec.2008.11.015
- Vaegter HB, Thinggaard P, Madsen CH, Hasenbring M, Thorlund JB. Power of words: influence of preexercise information on hypoalgesia after exercise-randomized controlled trial. Med Sci Sports Exerc. 2020;52(11):2373–2379. https://doi.org/10.1249/MSS.0000000000002396
- Chamsi-Pasha M, Albar MA, Chamsi-Pasha H. Minimizing nocebo effect: pragmatic approach. Avicenna J Med. 2017;7(4):139–143. https://doi.org/10.4103/ajm.AJM_59_17
- Peer RF, Shabir N. Iatrogenesis: a review on nature, extent, and distribution of healthcare hazards. J Fam Med Prim Care. 2018;7(2):309-314. doi: 10.4103/jfmpc.jfmpc_329_17. PMID: 30090769; PMCID: PMC6060929.
- Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Counsel. 2007;67(3):315–318. https://doi.org/10.1016/j.pec.2007.03.005
- Hall JA, Horgan TG, Murphy NA. Nonverbal communication. Annual Rev Psych. 2019;70:271–294. https://doi.org/10.1146/annurev-psych-010418-103145
- Ambady N, Koo J, Rosenthal R, Winograd CH. Physical therapists’ nonverbal communication predicts geriatric patients’ health outcomes. Psychol Aging. 2002;17(3):443–452. https://doi.org/10.1037/0882-7974.17.3.443
- Marletta G, Canfora A, Roscani F, Cernicchiaro L, Cutrera M, Russo M, et al. The complementary medicine (CAM) for the treatment of chronic pain: scientific evidence regarding the effects of healing touch massage. Acta Biomed. 2015;86 Suppl 2:127-33. PMID: 26629667.
- Tabatabaee A, Tafreshi MZ, Rassouli M, Aledavood SA, AlaviMajd H, Farahmand SK. Effect of therapeutic touch in patients with cancer: a literature review. Med Arch (Sarajevo, Bosnia and Herzegovina). 2016;70(2):142–147. https://doi.org/10.5455/medarh.2016.70.142-147
- Moseley GL. Placebo effect: reconceptualising placebo. BMJ. 2008;336(7653):1086. https://doi.org/10.1136/bmj.39577.518009.3A
- Davis CM. What is empathy, and can empathy be taught? Phys Ther. 1990;70(11):707–711. https://doi.org/10.1093/ptj/70.11.707
- Chaffey LJ, de Leeuw EJJ, Finnigan GA. Facilitating students’ reflective practice in a medical course: literature review. Educ Health (Abingdon). 2012;25(3):198–203.
- Aukes LC, Geertsma J, Cohen-Schotanus J, Zwierstra RP, Slaets JPJ. The effect of enhanced experiential learning on the personal reflection of undergraduate medical students. Med Educ Online. 2008;13:15.
About the Author(s)

Dustin Willis, PT, DPT
Dustin Willis PT, DPT is an Assistant Professor in the West Coast University Doctor of Physical Therapy program, where his focus is on teaching all the musculoskeletal content and injecting some of the humanities into healthcare through his Sociocultural Aspects of Human Interaction course. He is a Board-Certified Clinical Specialist in Orthopaedic Physical Therapy and a Fellow of the American Academy of Orthopaedic Manual Physical Therapists. When not in the classroom, he treats patients with Quantum Performance, a private concierge service provider that focuses on helping professional athletes to perform at the highest level possible. He is nearing completion of his dissertation, which is aimed at exploring the underlying psycho-neuro-endocrine-immunologic mechanism of providing compassionate care. Most importantly, he spends most of his time focused on raising his four-year-old medically complex, special needs son, Dorian Kahlil, who is the inspiration behind everything he does.

Everett B. Lohman III, DSc, PT
Everett B. Lohman III, DSc, PT is a professor at Loma Linda University (LLU), Post-professional and entry-level Doctor of Physical Therapy Programs, where his focus is on infusing humanities into the musculoskeletal curricular content. In his instruction, emphasis is placed on “whole patient care,” creating a healing alliance with patients through verbal and non-verbal communication, and the development of rapport and trust. He is a Board-Certified Clinical Specialist in Orthopaedic Physical Therapy. When not in the classroom, he serves as the Associate Dean for Graduate Academic Affairs and Assistant Dean for Research Affairs in the LLU, School of Allied Health Professions. He has published 100+ articles and routinely serves as a dissertation chair for PhD students. He is a masters lifting athlete and devoted father and grandfather. He enjoys spreading his passion for teaching whole-patient care (mind-body-spirit) nationally and internationally.

This work is licensed under a Creative Commons Attribution 4.0 International License.